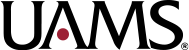
Dottie Lobbs (center) joins her physician, Muthu Veeraputhiran, M.D., (left) and husband Mike Lobbs at the first-ever UAMS Cancer Institute’s Celebration of Life. Lobbs underwent an allogeneic stem cell transplant at UAMS after being diagnosed with chronic myelomonocytic leukemia-2 .
Recovery from Acute Leukemia Gives Teacher Something to Celebrate
May 31, 2018 | It was the summer of 2015 and Dottie Lobbs should have been enjoying her summer break. Instead, Lobbs, a special education teacher at Glen Rose High School in Malvern, was experiencing such severe fatigue that she knew something was wrong.
It was probably bronchitis or some other easily treatable condition, her doctor said. But the antibiotics she was prescribed did not make a difference. As the first day of the new school year rolled around, Lobbs went back to the doctor and was quickly hospitalized. Still, however, no one could not determine the cause of her fatigue or abnormal blood work.
That’s when she asked for a referral to UAMS.
Within three days of her first appointment she was diagnosed with chronic myelomonocytic leukemia-2 (CMML-2), a type of cancer that starts in the blood-forming cells of the bone marrow and spreads to the blood.

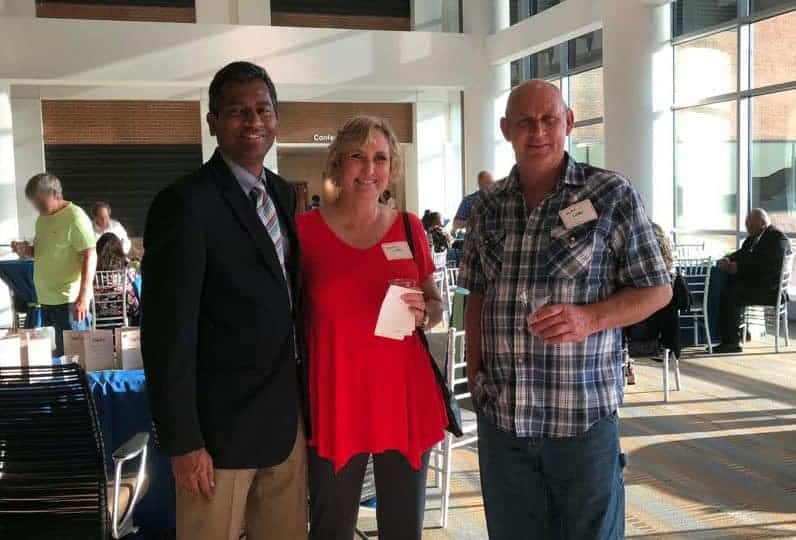
Allogeneic stem cell transplant patient Rhonda Young was joined at the event by Lane Johnson, her unrelated stem cell donor. Johnson traveled from Houston to attend the celebration.
“It was totally out of the blue,” she said.
While some other types of cancer are staged by the size of the tumor, CMML is split into two groups based on the percentage of immature cells, called blast cells, in the blood and bone marrow. In healthy people, blast cells make up 5 percent or less of normally developing marrow cells. In CMML-2, the percentage of blast cells is between 5 percent to 20 percent in the blood and 10 percent to 20 percent in the bone marrow.
With a team led by Muthu Veeraputhiran, M.D., director of the UAMS Allogeneic Stem Cell Transplant Program, Lobbs was admitted to the UAMS hospital Jan. 8 where she spent about the next 25 days undergoing her first round of chemotherapy.
“For patients who are diagnosed with acute leukemia and have high-risk features, we use chemotherapy to get them into remission while we search for a suitable stem cell donor,” said Veeraputhiran, who also is an associate professor in the UAMS College of Medicine Department of Internal Medicine.
An allogeneic stem cell transplant is the only curative treatment for CMML and requires a donation of blood-forming stem cells from another person. The first allogeneic stem cell transplant in the UAMS Winthrop P. Rockefeller Cancer Institute’s program was conducted May 13, 2015. “Our first transplant patient is still doing amazingly well today,” Veeraputhiran said.
UAMS has the only adult allogeneic stem cell transplant program in Arkansas and performs about 20 transplants per year for patients with acute leukemia and relapsed lymphoma. Veeraputhiran was named director of the program in February 2017.

About 60 guests attended the UAMS Allogeneic Stem Cell Transplant Program’s first-ever Celebration of Life on May 11.
Luckily for Lobbs, her brother was a suitable match and agreed to undergo the process to donate his stem cells to her.
Finding a stem cell donor is not always that easy, although research is improving the odds, Veeraputhiran said. Siblings have only a 25 percent match rate, and often people must turn to the national Be the Match stem cell donor registry to search for an unrelated donor.
A new process, however, can use donors who are a half-match, by incorporating novel combinations of therapies that minimize the rejection process.
For racial minorities, this is an especially important breakthrough, as African-Americans and Hispanics have less than a 30 percent chance of finding an unrelated donor through the national registry.
“The number of racial minorities in the registry is not as high as we would like it to be,” Veeraputhiran said. The unrelated match rate for whites is 60 percent to 70 percent due to higher rates of participation in the registry.
To prepare for his donation, Lobbs’ brother underwent four days of stem cell stimulating shots and had a port inserted into his chest for the blood to be drawn. Most stem cell donations are done through a blood draw.
While her brother was undergoing his preparation for the donation, Lobbs’ process was much more intense. After her first 25-day stay in the hospital, she went home for five days before returning to UAMS for 25 more. A 10-day round of outpatient chemotherapy followed, and, another 10-day stint in the hospital, culminating with her stem cell transplant on April 20.
After another 20 days in the hospital, she was released, but still had daily appointments at UAMS that required a one-hour drive back and forth from her home in the Brush Creek community outside Malvern.
Finally, on the 100th day after her transplant, Lobbs was declared cancer free. After easing back into the regular routine, she returned to work full time in December 2016.
“I had the most positive experience at UAMS that I possibly could have had. Dr. Veeraputhiran and his team were so wonderful. I am so grateful,” she said.
Even after having spent so much time at UAMS, Lobbs did not hesitate to accept an invitation to return on May 11, 2018, for an event honoring all of the patients who have undergone allogeneic stem cell transplants at UAMS, along with their donors and loved ones.
The program’s first-ever Celebration of Life welcomed about 70 people to the UAMS Cancer Institute to reminisce and reconnect over their shared experiences.
“I made a lot of friends while I was undergoing treatment, and it was good to see them,” Lobbs said, adding that visits from former transplant patients while she was hospitalized gave her hope that she would make it through as well. She hopes someday to pay it forward by volunteering with the program and offering living proof to patients that their disease can be overcome.
“Cancer is always scary, but acute leukemia and recurrent lymphoma are life-threatening emergencies. These patients beat the odds. We had this event to tell them we are honored to be part of their journey, and we believe their recovery is worth celebrating,” Veeraputhiran said.
In addition to Veeraputhiran, the transplant team includes physicians Pooja Motwani, M.D., and Appalanaidu Sasapu, M.D., both assistant professors in the UAMS College of Medicine Department of Internal Medicine; registered nurses, advanced practice registered nurses, case managers, social workers and staff of the UAMS hospital’s E7 wing and the UAMS Cancer Institute’s Infusion Clinic 4; and transplant coordinators.