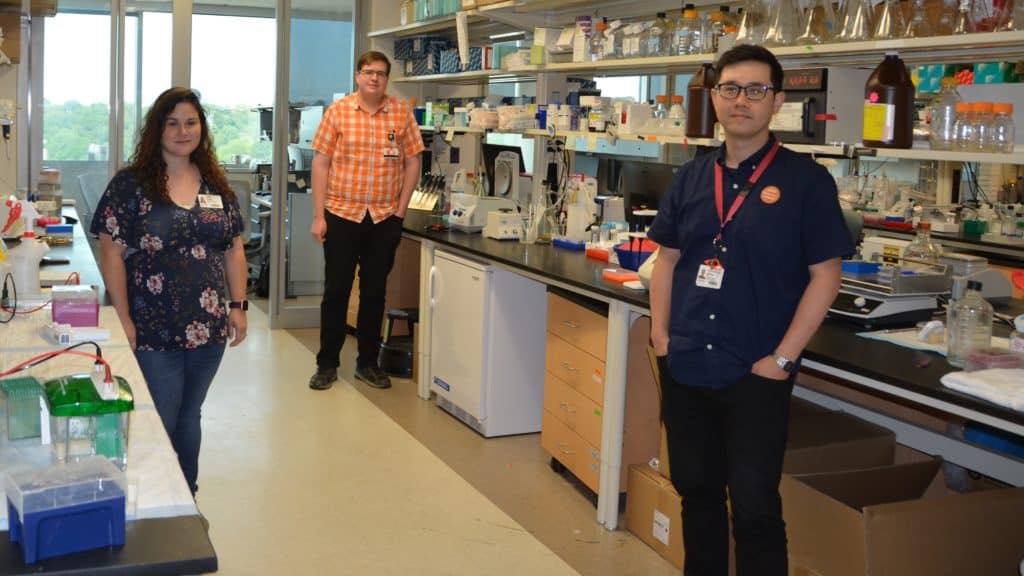
A UAMS research team led by Justin Leung, Ph.D., (pictured front) was published in the journal Nature Communications. Co-authors of the study are Jessica Kelliher, B.S., (left) and Kirk West, Ph.D.
Findings on DNA Damage Repair Published by UAMS Cancer Researcher
June 3, 2020 | LITTLE ROCK — A research team led by cancer researcher Justin Leung, Ph.D., at the University of Arkansas for Medical Sciences (UAMS) has uncovered the role of the protein RNF168 in DNA damage repair and shown how mutations of the protein affect people with a rare genetic condition.
The study titled “Histone H2A variants alpha1-extension helix directs RNF168-mediated ubiquitination” was published in the May 18 issue of the open-access journal Nature Communications.
“Every day our cells are subjected to environmental sources of DNA damage, such as ultraviolet radiation and toxic chemical exposure. If left unrepaired, these damages can accumulate, leaving mutations in our DNA and ultimately cause cells to become cancerous,” said Leung, assistant professor in the UAMS College of Medicine Department of Radiation Oncology.
In most cases, this damage is detected and repaired by a tightly regulated method involving many proteins. To develop better cancer therapies, researchers such as Leung strive to understand the regulation of DNA damage and repair by sensitizing cells to radiation therapy and chemotherapy drugs that target DNA.
“Our lab studies the repair of double stranded breaks, where both strands of DNA are broken apart completely. When a double strand break occurs, a cascade of protein activity is set off to try to resolve the damage,” Leung said.
Mutations in one of these proteins, RNF168, have been found in patients with RIDDLE syndrome, a rare genetic disorder that increases a person’s predisposition to blood cancer and is characterized by several attributes:
- Susceptibility to DNA damaging agents
- Immunodeficiency, or failure of the immune system to protect the body from infection
- Developmental abnormalities
- Learning disabilities
RNF168 adds a small signaling molecule called ubiquitin onto a subunit of chromatin, where we store our genetic information. The ubiquitin signal brings repair proteins to DNA double strand breaks. However, exactly how RNF168 recognizes the specific target remains unclear.
Using molecular and structural analysis methods, Leung’s team uncovered crucial components of RNF168 and chromatin required for the implementation of repair pathways in response to DNA damage. Their findings suggest that a recognition between RNF168 and chromatin is required to activate the downstream DNA repair processes.
“RNF168 is a central DNA damage response protein. Understanding the precise mechanisms by which it activates its targets is essential for understanding how the DNA damage response goes awry. Our results help demystify the role of RNF168 in proper DNA damage repair and understand the implications of RNF168 mutations such as those seen in RIDDLE syndrome,” Leung said.
UAMS authors for this study included Jessica Kelliher, B.S., research assistant, and Kirk West, Ph.D., postdoctoral fellow.
UAMS is the state’s only health sciences university, with colleges of Medicine, Nursing, Pharmacy, Health Professions and Public Health; a graduate school; a hospital; a main campus in Little Rock; a Northwest Arkansas regional campus in Fayetteville; a statewide network of regional campuses; and eight institutes: the Winthrop P. Rockefeller Cancer Institute, Jackson T. Stephens Spine & Neurosciences Institute, Harvey & Bernice Jones Eye Institute, Psychiatric Research Institute, Donald W. Reynolds Institute on Aging, Translational Research Institute, Institute for Digital Health & Innovation and the Institute for Community Health Innovation. UAMS includes UAMS Health, a statewide health system that encompasses all of UAMS’ clinical enterprise. UAMS is the only adult Level 1 trauma center in the state. UAMS has 3,275 students, 890 medical residents and fellows, and five dental residents. It is the state’s largest public employer with more than 12,000 employees, including 1,200 physicians who provide care to patients at UAMS, its regional campuses, Arkansas Children’s, the VA Medical Center and Baptist Health. Visit www.uams.edu or uamshealth.com. Find us on Facebook, X (formerly Twitter), YouTube or Instagram.###